IJDSIR : Dental Publication Service
Available Online at: www.ijdsir.com
Volume – 5, Issue – 3, June – 2022, Page No. : 515 – 520
Prognosis of a Polished Surface Basal Implant
Dr. Irfan Ali Motiwala, MDS Oral and maxillofacial surgery, Dr. Motiwala Dental clinic and Implant center, Hyderabad, Telangana, India.
Dr. Tejaswi Bathina, MDS, Oral Medicine and Radiology, Dr. Motiwala Dental clinic and Implant center, Hyderabad, Telangana, India.
Corresponding Author: Dr. Tejaswi Bathina, MDS, Oral Medicine and Radiology, Dr. Motiwala Dental clinic and Implant Center, Hyderabad, Telangana, India.
Citation of this Article: Dr. Irfan Ali Motiwala, Dr. Tejaswi Bathina, “Prognosis of a Polished Ssurface Basal Implant”,
IJDSIR- June – 2022, Vol. – 5, Issue – 3, P. No. 515 – 520.
Copyright: © 2022, Dr. Irfan Ali Motiwala, et al. This is an open-access journal and article distributed under the terms of the creative commons attribution non-commercial License. Which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Type of Publication: Case Report
Conflicts of Interest: Nil
Abstract
The macro and micro surfaces of dental implants have been modified over the years targeting better Osseointegration into the alveolar bone. Basal implants on the other hand utilize the concept of Osseo-fixation as a primary macro anchorage for the implants. They are later on osseointegrated in the alveolar bone. One of the important modifications of the surface of dental implants is the presence of a polished surface which greatly influences the risk of Peri-implantitis and therefore implants failure. This case report illustrates the prognosis and success rate of a olished surface basal implant, with a severe infection in the surrounding area.
Keywords
Basal implant, cortical implant, polished surface, osseo-fixation
Introduction
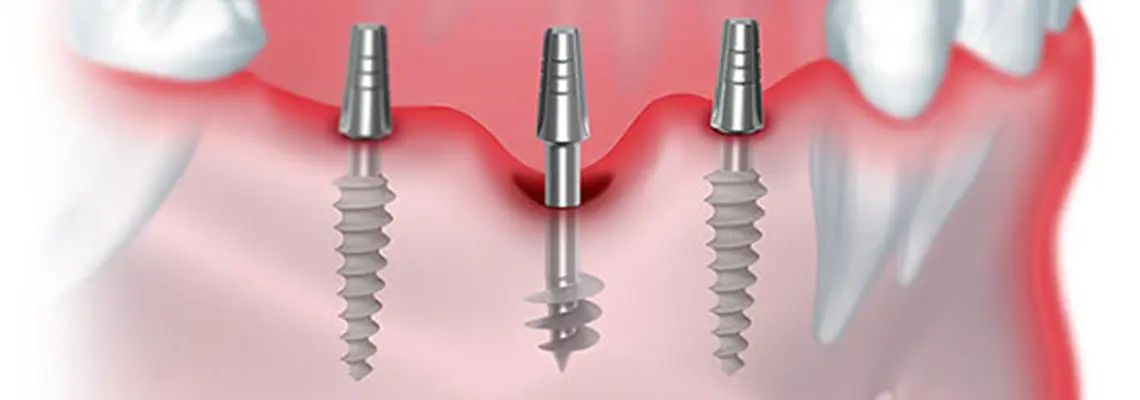
Basal implants utilize the concept of Osseo-fixation, by engaging the second or a third cortical bone which undergoes minimal or no resorption at all. This technique incorporates many advantages over the conventional crestal implants among which are great stability, avoiding additional surgical procedures in atrophic jaws (sinus lifting, bone grating), immediate loading of implants and low rates of implant failures are only a few1,2,3.
The polished surface of basal implants shows no response to inflammation. Hence in cases of sterile loosening of these implants, the polished surface helps in their reintegration, provided, the load is adjusted in time4,5,6.
Here, we are presenting a case report of a patient who has undergone full mouth rehabilitation with a combination of sandblasted and polished surface basal implants. The stability and success rate of these implants even with an infection in the adjacent area is clearly depicted in this report.
Case Report
A 57-year-old female patient came to the clinic with a chief complaint of missing teeth in the upper and lower front and back teeth region for two years. Her history revealed a previous visit to one of the local dentists, on whose suggestion, got all of her teeth extracted so as to get full mouth rehabilitation. Informed about various methods in which the teeth can be replaced, she considered getting implant-supported complete dentures done. The dentist apparently placed a bone graft following extractions, to accommodate for the implants and advised me to come after three months.
Present clinical examination revealed well-developed ridges with no excessive resorption and good depth of the vestibule. After discussing the entire procedure and other modes of replacing teeth, the patient opted to get a full-mouth fixed prosthesis using basal implants. Her medical history was non-contributory with no systemic problems. A preliminary panoramic radiograph was taken to determine the bone level in both jaws. The radiograph showed completely edentulous upper and lower arches except for a root piece in relation to the lower left quadrant. The peri-apical region bordering the root piece however did not show any radiolucency, instead had a well-formed bone over it. Considering the absence of any clinical or radiological pathosis, and well-formed bone around it, the root piece was left as such and the patient was informed about it.
A pre-operative cone beam computed tomography was taken to evaluate the quality and quantity of the bone along which implants are to be placed. A combination of sandblasted and polished surfaced single-piece basal implants (12 in the upper arch and 10 in the lower arch) were placed in both jaws with minimal trauma under local anesthesia using a flapless technique. The implants on the lower left quadrant were placed in such a manner, that they are not in close proximity to the root piece. Temporization was done and the patient was sent after giving all the post-operative instructions. On the second postoperative day, a coping trial was done to accommodate the zirconia bridge. Tentative occlusal records were taken using jet bite. The final trial was made to adjust the anatomy of the teeth and the prosthesis was fixed on the third postoperative day. High points were removed and occlusion was adjusted. Excess cement, if any, was removed and all the post-operative instructions were given. The patient was followed up after every 3 months.
The patient did not have any complications until one year, after which she noticed mild tenderness in the lower left quadrant which was intermittent, throbbing type and sometimes associated with swelling. The swelling and the pain would subside on taking medication, but only to recur after a few days. On seeking a radiograph, the OPG revealed a radiolucency surrounding the root piece. Assuming a possible infection of the root piece and a consequent implant failure, the patient was given an appointment to approach the clinic.
On clinical examination, the patient had tenderness in the posterior region of the lower left back tooth region. There was a deep pocket with pus discharge adjoining the last implant in the lower left quadrant, which was, however, not associated with any mobility. No pain or discomfort was noted while percussing any of the implants. The zirconia bridge was removed to clearly analyze the implants. On a thorough check-up of the implants, none of them were found mobile.
The patient was explained about the infection around the root piece and was advised to get that removed. Starting an antibiotic course (Augmentin 625mg twice daily), the root piece was removed on the following day under local anesthesia. The surrounding area was meticulously curettaged to remove all the granulation tissue. The implant was re-examined to check for mobility and/or tenderness but none were noted. Localized antibiotic therapy using minocycline 1mg (Arestin) was administered by placing them in the socket. Temporization was done until the final zirconia bridge was cemented. Necessary medication and instructions were prescribed. The final zirconia bridge was then fixed after a week, making sure that the extraction site is properly healed. The patient is under constant follow up and the radiograph after four months showed good bone formation around the implant with no evidence of any pathology.
Discussion
Fate of Retained Root Piece
Extraction of teeth can be advised in a variety of dental conditions. The prevalence of retained root pieces in dentulous or edentulous patients is considered to be one of the common findings in radiographic examinations. The root piece left behind by the previous dentist, in our case report, was asymptomatic with no evident pathology detected in the radiograph. Literature has provided diverse opinions on deciding whether or not to remove a broken tooth fragment in the jaws. According to the submerged root concept, a fractured tooth with no pathology will apparently not cause any infection in the future. Also, tooth fragments present near the surface of the alveolar socket are extruded by the epithelial lining during socket healing. However, when they are deeply placed inside the socket, they are not extruded but bone forms around them as a part of the healing process. It also presumably helps in reducing the rate of alveolar bone resorption to some extent7, 8, 9. As far as our case is concerned, the root piece was deeply seated with a good amount of bone surrounding the root piece and no pathological changes were detected either clinically or radiographically. Hence, the patient was informed about the root and was left as such, avoiding traumatic extraction of the submerged root.
Choosing a polished surface over a rough surface The surface roughness of conventional implants is usually in the range of millimeters to microns10. This rough surface, engaging the alveolar bone, primarily targets Osseo-integration by aiding bone formation between those surface irregularities. However, surface modification of implants results in creating a more rough surface, which provides a suitable opportunity for plaque and bacterial accumulation and therefore more prone to peri-implantitis11. Hence, in conditions like this, where a probable infection surrounds the implant, there is a higher chance that the granulation tissue and bacteria harbour these minute gaps making it impossible to eliminate the entire lesion. Although sandblasted implants aid in acquiring better osseointegration, as a result of their surface roughness, polished surface basal implants are best chosen in conditions where there is a potential for infection. Some of these conditions are chronic periodontitis, placing implants after immediate extraction of teeth, and cases with retained root pieces in the bone.
In a rough surface crestal implant, this level of infection might have resulted in Peri-implantitis. The microbial biofilm plays a major role in the onset and progression of Peri-implantitis. Hence the treatment mainly targets removing the biofilm which can be done by mechanical debridement or Implantoplasty. This procedure is targeted at eliminating the bacterial biofilm through smoothening/polishing the implant surface and/or contouring the bone12. Peri-implantitis with more than 2mm of bone loss require surgical management in addition to mechanical debridement and antibiotic therapy. In conditions where more than half of the implant length is infected, it indicates implant failure and hence should be removed13.
The present case report showed a considerably large lesion around the implant with a probing depth of more than 4mm, bleeding with suppuration, and a radiolucent lesion of around 10mm x 8mm in diameter involving almost more than half of the implant. But, the polished surface and primary anchorage in the infection-free basal bone, contributed greatly to the success of the implant. The polished surface of the implants inherently shows very less or no response to inflammation which is clearly evident in our present report. The absence of surface roughness eliminates the micro gaps reducing bacterial colonization thereby increasing the chance of eliminating the infection completely. This smooth, polished surface and the self-incorporated abutment, completely remove the interface problems and therefore peri-implantitis5,6. Thus we have considered using a polished surface single-piece implant in this area.
Advantage of Acquiring Anchorage from The Cortical Bone
Another important concern while restoring teeth with implants is implant stability. In the case of full-mouth rehabilitation, single-piece implants are used at our centre. The prosthesis is fixed in three consecutive appointments, utilizing the concept of immediate loading (Permanent Teeth in 3 Days). Basal implants acquire great primary stability utilizing the concept of Osseofixation. They are anchored into the basal bone which is usually infection free and has minimal or no resorption at all6,7. The cortical bone shows a lower metabolic rate when compared to the alveolar bone. Thus when these basal implants are immediately loaded and adequate occlusal forces are equally distributed along the bone, not only a great primary stability is achieved, but there is also an increased formation of bone around the implant corresponding to Wolff’s law of bone remodeling.
The present case report shows that even though the retained root piece was relatively vital and deeply seated with bone formation around it, there was a consequential formation of a lesion suggesting a foreign body reaction. This also suggests that the radiograph showed a prominent radiolucency almost nearing the adjacent implant implying its apparent failure. However, the clinical examination did not show any signs of implant failure. This observation highlighted the prognosis and the success rate of using a polished surface single-piece basal implant. Had it been a conventional rough surface multiunit implant, there is a greater chance of the occurrence of Peri-implantitis and an apparent implant failure. The prominent lesion in the alveolar part of the bone and the rough surface of conventional implants limiting the complete elimination of the infection would have led to its failure. This also suggests that basal implants acquire great anchorage from the highly stable cortical bone through Osseo fixation. Even minimal thickness of cortical bone (as low as 2.5mm in the present report) is adequate for the success of implants and can be successfully placed in patients with atrophic jaws.
Conclusion
The present case report highlights the success rate of using a polished surface basal implant in restoring missing teeth. Engaging second or third cortical plates through the use of basal implants not only gives great primary stability but the polished surface remains immune to infection in the surrounding area. Extreme care must however be taken while placing them so that the cortical bone is properly engaged and any damage to the adjacent vital structures is eliminated.
References
1. Shakhawan MA, Zanyar MA, Rebwar AH, Haw bash OM, Rozhyna PK, PaymanKh M. All-On-Four Treatment Concept in Dental Implants: A Review Articles. Sur Cas Stud Op Acc J. 2(4)- 2019. SCSOAJ. MS. ID. 000142. DOI: 10.32474 / SCSOAJ. 2019. 02. 000142.
2. Safii SH, Palmer RM, Wilson RF. Risk of implant failure and marginal bone loss in subjects with a history of periodontitis: A systematic review and metaanalysis. Clin Implant Dent Relat Res. 2010; 12:165–74
3. Ali, S.M., Mahmud, P. Kh., Othman, K.S. and Samad, A.A. (2019) Single Piece Dental Implant: A Remedy for Atrophic Ridges: Review. International Journal of Otolaryngology and Head & Neck Surgery, 8, 271-282. https :// doi .org/ 10. 4236/ ijohns. 2019. 86025.
4. Aakarshan Dayal Gupta, Avira Verma, Tanay Dubey, Saloni Thakur. Basal osseointegrated implants: Classification and review. International Journal of Contemporary Medical Research 2017;4(11):2329-2335.
5. Yadav RS, Sangur R, Mahajan T, Rajanikant AV, Singh N, Singh R An Alternative to Conventional Dental Implants: Basal Implants. Rama Univ J Dent Sci 2015 June;2(2):22-28.
6. Ihde, S. (2009) Comparison of Basal and Crestal Implants and Their Modus of Application. Smile Dental Journal, 4, 36-46.
7. Nayyar, Junaid& Clarke, Mary & O’Sullivan, Michael & Stassen, Leo. (2015). Fractured root tips during dental extractions and retained root fragments. A clinical dilemma? British dental journal. 218. 285-290. 10.1038/sj.bdj.2015.147.
8. Casey DM, Lauciello F R. A review of submergedroot concept J Prosthet Dent 1980; 43:128-132R.
9. Von Wowern, N., &Winther, S. (1981). Submergence of roots for alveolar ridge preservation. International Journal of Oral Surgery, 10(4), 247–250. doi:10.1016/s0300-9785(81)80066-x
10. K. Alla, K. Ginjupalli, N. Upadhya, M. Shammas, R. Krishna Ravi, and R. Sekhar, “Surface roughness of implants: a review,” Trends in Biomaterials and Artificial Organs, vol. 25, no. 3, pp. 112–118, 2011.
11. Mahato, Nisha& Wu, Xiaohong& Wang, Lu. (2016). Management of peri-implantitis: a systematic review, 2010–2015. Springer Plus. 5. 10.1186/s40064-016-1735-2.
12. Smeets, R., Henningsen, A., Jung, O. et al. Definition, etiology, prevention and treatment of periimplantitis – a review. Head Face Med 10, 34 (2014). https :// doi. org/10.1186/1746-160X-10-34
13. Carrasco-García A, Castellanos-Cosano L, Corcuera-Flores JR, Rodríguez-Pérez A, Torres-Lagares D, Machuca-Portillo G. Influence of marginal bone loss on peri-implantitis: Systematic review of literature. J Clin Exp Dent. 2019; 11 (11): e1045 – e1071. Published 2019 Nov 1. doi: 10.4317 / jced. 56202
Supplementary Data Description
1. Image showing preoperative OPG
2. Preoperative CBCT image
3. Implant placed far away from the root piece
4. CBCT image of the lesion
5. Clinical Picture of the lesion
6. CBCT image after extraction
7. Follow up Radio graph